Chugai Pharmaceutical Co., Ltd. issued the following announcement on Oct. 30.
- NMOSD is a rare disease where repeated relapses may result in visual impairment and motor disability in the course of disease progression.
- The applications are based on the results from two positive global phase III studies evaluating satralizumab monotherapy and add-on therapy to baseline immunosuppressant therapy.
- The applications will be reviewed under Accelerated Assessment by EMA.
“NMOSD is a disease with high unmet medical needs, which causes visual impairment and motor disability in the course of disease progression,” said Dr. Yasushi Ito, Chugai’s Executive Vice President, Co-Head of Project & Lifecycle Management Unit. “Satralizumab is the investigational medicine that has demonstrated a clinically meaningful treatment effect as both monotherapy and add-on therapy to baseline treatment. We are collaborating with Roche and regulators to deliver this new treatment option to patients as soon as possible.”
Accelerated Assessment reduces the timeframe for the EMA and CHMP to review the marketing authorization, signifying the treatment is of major interest for public health and therapeutic innovation. These applications are based on the results from global phase III clinical studies in patients with NMOSD: SAkuraStar Study (NCT02073279) evaluating satralizumab monotherapy, and SAkuraSky Study (NCT02028884) evaluating satralizumab added to baseline treatment.
About satralizumab
Satralizumab, created by Chugai, is an anti-IL-6 receptor recycling antibody. The drug is expected to suppress relapse of NMOSD by inhibiting IL-6 signal transduction which is deeply related to the pathology. In two global phase III clinical studies in neuromyelitis optica (NMO) and NMOSD patients, the primary endpoint was achieved with satralizumab either as an add-on therapy to baseline treatment (NCT02028884) or as monotherapy (NCT02073279). These studies represent one of the largest clinical trial programs undertaken for this rare diseases. Satralizumab is designated as an orphan drug for the treatment of NMO and NMOSD in Japan, and for the treatment of the same disease group in Europe and the U.S.. In addition, it has been granted Breakthrough Therapy Designation by the U.S. Food and Drug Administration in December 2018.
About neuromyelitis optica spectrum disorder (NMOSD)
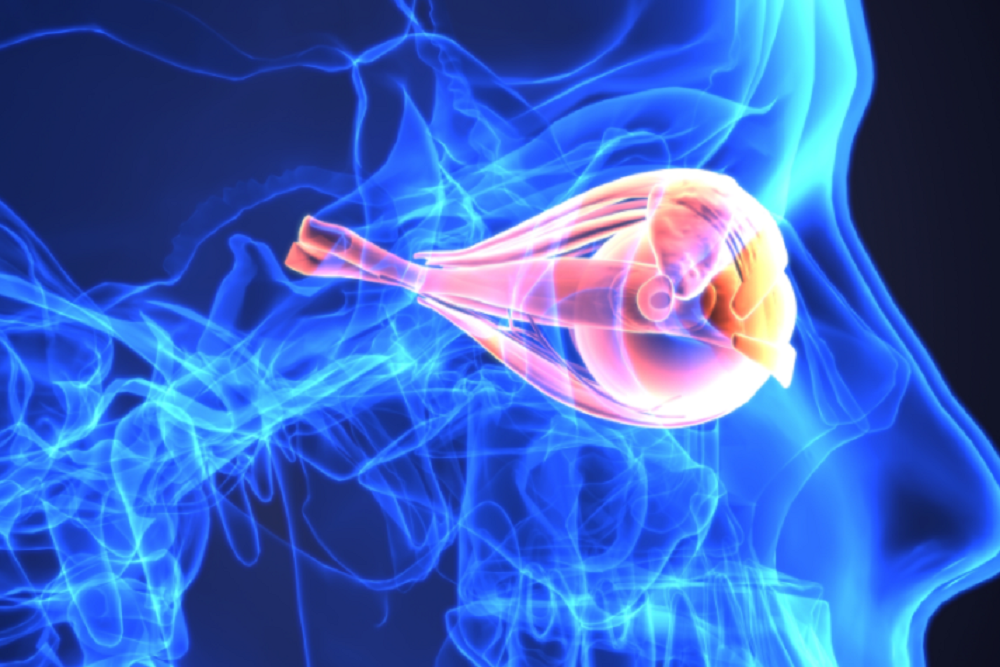
NMOSD is a rare, lifelong, and debilitating autoimmune disease of the central nervous system (CNS) characterized by inflammatory lesions in the optic nerves and spinal cord. Patients with NMOSD frequently experience a relapsing disease course with repeated attacks leading to accumulating neurological damage and disability. Symptoms may include visual impairment, motor disability, and loss of quality of life. In some cases, attacks of NMOSD result in death. NMOSD is commonly associated with pathogenic antibodies (AQP4-IgG) that target and damage a specific central nervous cell type called astrocytes, resulting in inflammatory lesions of the optic nerve(s), spinal cord and brain. AQP4-IgG are detectable in the blood serum of around two-thirds of NMOSD patients. The inflammatory cytokine IL-6 is now emerging as an important factor in NMOSD pathogenesis.
Diagnostic criteria introduced in 2006 for NMO were characterized by inflammation of the optic nerve (optic neuritis) and the spinal cord (myelitis). These were revised in 2007 with the definition of NMOSD, proposed for diseases with either optic neuritis or myelitis. In 2015, the definition of NMOSD further revised to include a broader spectrum of disease. The diagnostic term NMOSD is now widely used.
Sources




